If you have hypermobility spectrum disorder (HSD) or Ehlers-Danlos syndrome (hEDS), you may have experienced unexpected complications with surgery or anesthesia. These aren’t just bad luck – they’re often directly related to your hypermobility condition. Understanding why these issues occur and what you can do about them can help you advocate for better surgical care and potentially prevent problems in the future.
The Story Behind This Guide

A collaboration between Sharon Hennessey (Not Just Bendy Hypermobility Services), Dr. Jason Lam (The Dance Dr), and Bianca Comfort (Comfort Psychology) has produced a comprehensive Peri-Operative Management of Patients with Hypermobility, Mast Cell Activation Syndromes and Dysautonomia (the “Trifecta”) specifically for medical professionals. This evidence-based resource has been featured on the Mayo Clinic EDS blog and the Ehlers-Danlos Society, giving healthcare providers the tools they need to safely care for hypermobile patients during surgery.
But we realized that while having a medical guide was crucial, our clients needed their own version – one that explained these complications in plain language and gave them practical strategies to advocate for themselves. That’s why we created this patient-friendly guide, directly addressing the most common complaints we hear from people with hypermobility about their surgical experiences.
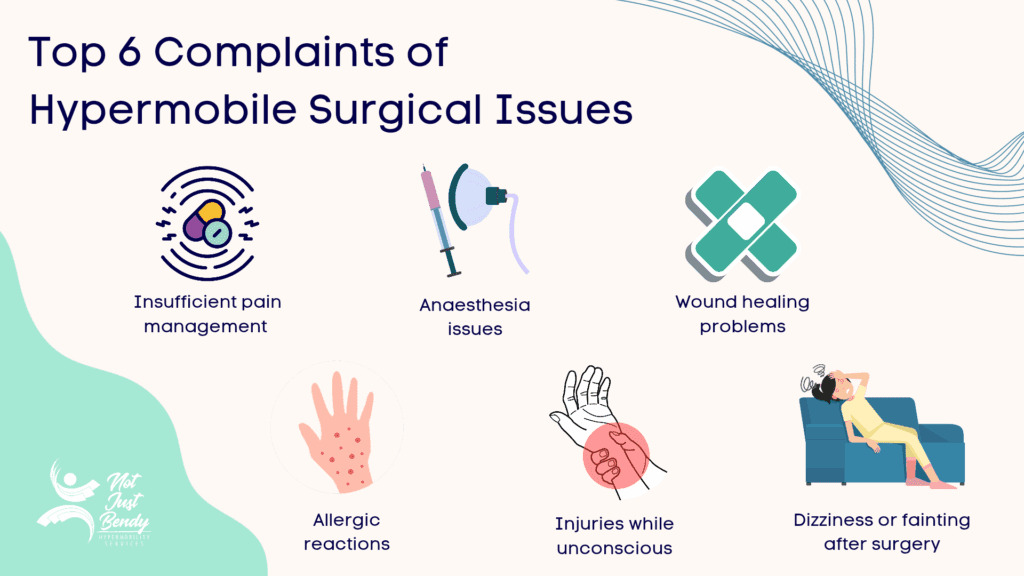
1. “Why didn’t my anesthetic or pain relief work properly?”
Why this happens in hypermobility: Your connective tissue differences affect how local anesthetics are absorbed. Lidocaine often doesn’t work properly in hypermobile people – this is a real physiological difference, not psychological.
What can be done:
- Ask for articaine or bupivacaine instead of lidocaine (3-4x more effective)
- Consider regional blocks or general anesthesia for larger procedures
- Document previous anesthetic failures in your medical records.
2. “Why did I have a mast cell reaction during/after surgery?”
Why this happens in hypermobility: Mast Cell Activation Syndrome is common with hypermobility. Surgery stress, certain medications, temperature changes, or IV preservatives can trigger inappropriate mast cell activation.
What can be done:
- Continue your usual antihistamines (H1 and H2) until surgery
- Ask to avoid histamine-releasing drugs (atracurium, mivacurium, nefopam)
- Request preservative-free preparations when possible
- Ask for temperature control and warmed blankets
3. “Why did I faint or feel awful when I tried to get up after surgery?”
Why this happens in hypermobility: 90% of hypermobile people have orthostatic intolerance – difficulty maintaining normal blood pressure and heart rate when upright. Surgery and bedrest worsen this significantly. Learn more about POTS and orthostatic intolerance here.
What can be done:
- Ask for baseline lying/standing vital signs before surgery
- Request liberal IV fluids before, during, and after surgery
- Insist on very slow position changes (lying→sitting→standing)
- Expect longer mobilization times – don’t rush recovery
4. “Why didn’t my wound heal properly or why did I bleed so much?”
Wound Healing Problems in hEDS
Why this happens in hypermobility: Your connective tissue differences cause fragile blood vessels and slower healing. Mast cell activation can also increase bleeding risk. Wounds can reopen weeks later when you think everything’s fine.

What can be done:
- Discuss bleeding concerns – ask about tranexamic acid or DDAVP
- Request stronger closure techniques (dual-layer sutures, PDS/Maxon)
- Ask for extended Steristrip use (6 weeks instead of 1-2 weeks)
- Plan for longer healing times and report wound concerns promptly
5. “Why did my neck pain start or get worse after surgery?”
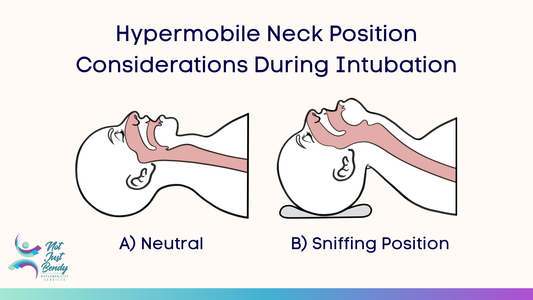
Why this happens in hypermobility: Cervical instability is common but often unrecognized. During anesthesia, your neck loses muscle protection and can be positioned unsafely. Standard intubation can stress unstable joints.
What can be done:
- Inform the team about neck pain or TMJ issues
- Ask for rheumatoid arthritis-style airway management
- Request fiber-optic intubation – as neck can stay in a straight position (A). Normal intubation places the neck into extension (or the sniffing position) (B)
- Take a soft or hard neck collar with you to surgery as a visual and physical reminder
- Ask for careful positioning and post-operative neck support
6. “Why did my joints injure or sublux during surgery?”
Why this happens in hypermobility: Under anesthesia, you lose muscle tone that protects hypermobile joints. Standard positioning and transfers can cause subluxations or dislocations.
What can be done:
- Speak with nursing staff before surgery about your joint issues
- Ask to self-position initially before anesthesia
- Request extra joint padding and support during transfers
- Ask if supportive braces can stay on during surgery
- Specify which joints are most problematic
7. “Why didn’t anyone listen to my concerns about my hypermobility?”
Why this happens in hypermobility: Many healthcare providers have limited training about hypermobility disorders and may not understand your legitimate medical concerns.
What can be done:
- Bring written documentation of your diagnosis
- Ask your specialist to write a letter about surgical risks
- Request a pre-op meeting specifically about hypermobility concerns
- Ask direct questions about how they’ll address your needs
- Don’t hesitate to seek a second opinion if dismissed
Moving Forward: You Have the Right to Safe Surgery
These surgical complications are not something you have to accept as “just part of having hypermobility.”
By understanding why they occur and knowing what to ask for, you can work with your medical team to prevent many of these issues. Remember – your concerns are valid and based on real physiological differences.
For more information and to access our comprehensive perioperative management guide for your medical team, click here to download the PDF.
We’ve collated evidence and experience from a wide range of sources to create suggestions for surgical teams, drawn from those working with hypermobile patients daily.

Want To Learn More From Sharon Hennessey About Hypermobility?
Sharon’s ground-breaking hypermobility educational courses through The Hypermobility Project are launching soon – sign up now to know when the courses go live!
Join the wait list to be the first to access exclusive video content, tailored for health professionals seeking to better understand hypermobility.
Learn More
You can find more information curated by Not Just Bendy at:
- What Is Hypermobility?
- Mast Cell Activation Disorders
- Postural Orthostatic Tachycardia Syndrome (POTS)
- Exercise Tips for Postural Orthostatic Tachycardia Syndrome (POTS)
- Hypermobile Hips
- Women’s Health Issues In Hypermobility
- Switching on the Lightbulb to see Hypermobility Disorders
- Hypermobility Screening & Prevention
- Exercise Classes for Hypermobility
- Hypermobility Resources
- Hypermobility Brisbane Physiotherapy
References
Anderson, Linda K. “CE: Nursing Management of Patients with Ehlers-Danlos Syndrome.” The American Journal of Nursing 115, no. 7 (2015): 38–46; quiz 47–48. https://doi.org/10.1097/01.NAJ.0000467274.82951.57.
Hakim, Alan J, Rodney Grahame, Paul Norris, and Colin Hopper. “Local Anaesthetic Failure in Joint Hypermobility Syndrome.” Journal of the Royal Society of Medicine 98, no. 2 (2005): 84–85. https://doi.org/10.1177/014107680509800222.
Johnston, Barrett A., Kaitlin E. Occhipinti, Amir Baluch, and Alan D. Kaye. “Ehlers-Danlos Syndrome: Complications and Solutions Concerning Anesthetic Management.” Middle East Journal of Anaesthesiology 18, no. 6 (2006): 1171–84. https://pubmed.ncbi.nlm.nih.gov/17263273/
Ramírez-Paesano, Carlos, Albert Juanola Galceran, Claudia Rodiera Clarens, et al. “Opioid-Free Anesthesia for Patients with Joint Hypermobility Syndrome Undergoing Craneo-Cervical Fixation: A Case-Series Study Focused on Anti-Hyperalgesic Approach.” Orphanet Journal of Rare Diseases 6, no. 172 (2021): https://doi.org/10.1186/s13023-021-01795-4
Russek, Leslie N., Nancy P. Block, Elaine Byrne, et al. “Presentation and Physical Therapy Management of Upper Cervical Instability in Patients with Symptomatic Generalized Joint Hypermobility: International Expert Consensus Recommendations.” Frontiers in Medicine 9 (January 2023). https://doi.org/10.3389/fmed.2022.1072764.
Wiesmann, Thomas, Marco Castori, Fransiska Malfait, and Hinnerk Wulf. “Recommendations for Anesthesia and Perioperative Management in Patients with Ehlers-Danlos Syndrome(s).” Orphanet Journal of Rare Diseases 9, no. 1 (2014): 109. https://doi.org/10.1186/s13023-014-0109-5.
